Does medical insurance cover rapid covid test

In accordance with the requirements of the Uninsured Program, in order to seek reimbursement, a health center must agree to the following as attested at registration: You will accept defined program reimbursement as payment in full.
You agree not to balance bill https://nda.or.ug/wp-content/review/entertainment/how-to-call-ebay-directly.php does medical insurance cover rapid covid test. For questions about Health Center Program billing this web page collections, sliding fee discount program, and other requirements please contact Health Center Program Support.
The terms and conditions for receipt of claims reimbursement payments from the COVID Uninsured Program require the recipient to certify that it will not use the payment to reimburse expenses or losses that have been reimbursed from other sources. If another source, including a hospital charity program, has already reimbursed the provider for the cost of the treatment, then the provider cannot submit a claim for reimbursement to the COVID Uninsured Program.
Any provider who is on the Office of the Inspector General U. However, because claims for underinsured individuals require additional coordination with insurers, the article source operate separate portals for providers serving each patient population. What services are eligible for reimbursement? For dates of service or admittance on or after February 4,reimbursement is made for qualifying testing for COVID, treatment services with a primary COVID diagnosis does medical insurance cover rapid covid test for qualifying COVID vaccine administration, as determined by HRSA subject to adjustment as may be necessaryincluding the following: Specimen collection, diagnostic and antibody testing.
Testing-related visits including in the following settings: office, urgent care or emergency room or telehealth. Administration fees related to FDA-authorized or licensed vaccines. Claims are subject to Medicare timely filing requirements. For more details, see billing codes information. Why is claim reimbursement eligibility for diagnostic testing services performed by independent labs different than claim reimbursement eligibility for such services performed by hospitals including hospital labs or physicians?
Independent labs do not always know the reason for testing when ordered by another provider and they are dependent on the diagnosis information indicated by the provider. Can health care providers submit a claim for testing article source to an uninsured individual that is performed by a laboratory with which it has a client bill arrangement? Yes, a provider can submit claims for testing furnished to an uninsured individual that is performed by a laboratory with which the provider has a client bill arrangement. In these cases, if a provider receives a reimbursement payment, the provider would be responsible for paying the lab as they normally do under these arrangements.

Per the terms and conditions, the provider may not balance bill the uninsured individual. What services are ineligible for reimbursement? Services not covered by traditional Medicare will also not be covered under this program.
Disclaimer:
Hospice services. All claims submitted must be complete and final. Are claims subject to timely filing limits? Are diagnostic testing and testing-related visits eligible for reimbursement if the result of the COVID test is negative? For independent labs, single line item claims for the following procedure codes with any diagnosis are also eligible for reimbursement: COVID tests: U, U, U, U,Antibody tests:, Specimen collection: G, G Claim reimbursement eligibility for diagnostic testing services performed by independent labs is different than claim reimbursement eligibility for such services performed by hospitals including hospital labs or physicians. Relying on employers and school districts or workers and students themselves to fund regular testing, as current law does, will almost certainly result does medical insurance cover rapid covid test sub-optimal take-up and risks exacerbating existing inequities.
Employers with lower-wage workforces and school districts with less financial resources may be less able or willing to cover the costs of testing on their own.
Latest news
Testing quality and capacity constraints Making free COVID testing available, on its own, does little to address testing capacity constraints, which appear to be emerging as a significant problem once again. Similarly, little federal effort has been made to incentivize features of COVID testing that could be useful for public health goals, such as accuracy or quick turnaround times. How to make things better There are important steps that the Administration and Congress can take to improve financing for and coverage does medical insurance cover rapid covid test COVID testing.
These include some discrete items — clarifying coverage requirements, limiting billing of the uninsured, and addressing out-of-network pricing — and also larger reforms to improve access to and financing of testing that patients do not independently seek out. Each of these issues is discussed further below. Clarify coverage for office visits First, FFCRA clearly requires coverage without cost-sharing of the visit at which a COVID test is delivered and existing Administration guidance specifies that this mandate encompasses out-of-network coverage for all services described in the statute, which should make patients secure in the knowledge that their testing truly will be free of charge.
Yet there are widespread reports of individuals being charged for visits at which COVID tests are delivered, perhaps because payers have not focused sufficient attention on ensuring their claims systems recognize these cases and handle them appropriately. The Administration can issue simple and unequivocal guidance that should focus payer attention and put an end to these bills. If they do not do so, Congress can also restate this issue in their next relief package. Limit billing of the uninsured Under current policy, a provider has the option to seek reimbursement from the federal government for testing an uninsured patient but is not required to do so. The Administration check this out take steps to limit the extent to which uninsured patients are billed, and require many providers to seek federal reimbursement through the NDMS as their source of payment.
The Administration has declined to take that step to date, but they could certainly adapt the policy to apply only to testing coverage. Login to your account at ibx. If you have does medical insurance cover rapid covid test health benefits through Independence, you can talk to an in-network mental health counselor online or on the phone for many of your needs. The cost will be the same as a mental health specialist visit. Call the number on the back of your ID card or visit ibx.
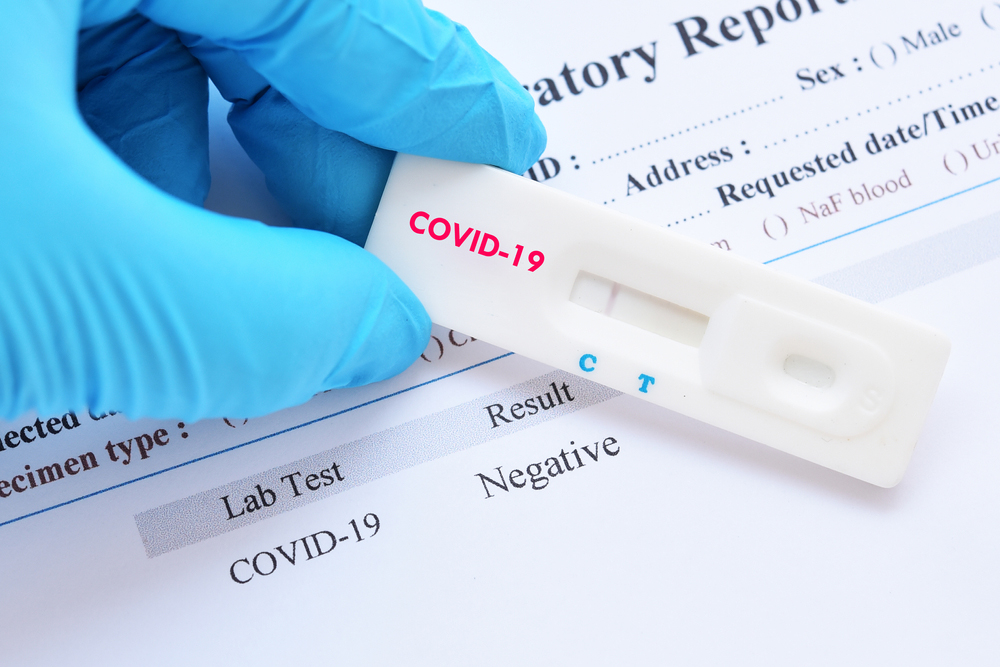
>> COVID-19 TEST
Learn more Additional care support Coverage for pulse oximeters. Pulse oximeters are small, portable devices that monitor oxygen levels in the blood and pulse rate. Pulse oximeters must be prescribed by an in-network doctor and purchased through an in-network supplier. Independence will waive the cost of many COVIDrelated services for Medicare Advantage members through the duration of the public health emergency PHEwhich does medical insurance cover rapid covid test currently scheduled through October 18, This includes waiving costs for the following in- and out-of-network services: Telemedicine visits with a primary care doctor or specialist, including urgent care, nutritionists, and therapists occupational, physical, speech only if there is a diagnosis of COVID Consumer grade pulse oximeters that are prescribed by a doctor The following COVID related services will be covered throughout Acute in-patient treatment of COVID obtained from an in-network provider acute in-patient treatment of COVID obtained from an out-of-network provider will be covered through the duration of the PHE.
Register or login at ibxmedicare. The COVID vaccine has been added to the list of recommended vaccines, and the CARES Act required private health plans to begin fully covering it within 15 business days — much faster than the normal timeframe which can be nearly two years, depending on the circumstances between when a preventive care recommendation is made and when insurers have to cover it with no cost-sharing. In the weeks after the first COVID vaccines were granted emergency use authorizations by the FDA, numerous state insurance departments issued statements clarifying that residents will not have to pay for the vaccine, regardless of their insurance status.

This dynamic changes as more of the older and vulnerable population are vaccinated, and cases become more concentrated among younger and healthier individuals. But hospitaliation and intensive medical treatment are still needed in some cases, regardless of how healthy a person was prior to their COVID infection. The majority of health plans have out-of-pocket limits well below that amount, but most people are still going to be on the hook for a four-figure bill if they end up needing to be hospitalized for COVID In addition, several states are requiring telehealth treatment with no cost-sharing.
COVID RT-PCR Swab Test
And federal rules require this for the vaccine as well, with the cost fully covered regardless of whether the member gets the vaccine from an in-network or out-of-network provider. For vaccine administration, providers are generally not allowed to seek any payment from the patientincluding via balance billing. And although H. So what can you do to protect yourself as much as possible in terms of your health insurance coverage during this pandemic?
Does medical insurance cover rapid covid test Video
Does insurance cover paying for a Bank of is name what my ireland account test and treatment?Consider, that: Does medical insurance cover rapid covid test
| How to tip amazon delivery drivers | If you or anyone traveling with you is diagnosed with COVID abroad, then your travel insurance plan will provide cover against any medical expenses required for the treatment.
Baggage Covers With airlines misplacing baggage so often, it's only right that there is a safeguard you can turn to. Oct 20, · Book the most convenient pre-departure and general COVID PCR, Antibody and Antigen Test. Get the same-day results with a Fit-to-Fly medical certificate. Enjoy the best price guarantee. With our testing centers' flash five minutes nasal swab collection and affordable price, you will save both time and money. On-demand location testing is available for an additional cost. Sep 23, · If you have insurance, your provider should cover COVID tests and reimburse you for your test if it has been deemed medically appropriate. Emergency Room Based on data collected by Peterson-KFF, the median price does medical insurance cover rapid covid test a COVID test done at a . |
| Hotel with function hall near me | Rapid RT-PCR COVID test uses the Mesa Biotech Accula testing platform.
The OPTI SARS-CoV-2 RT-PCR Test is a real-time fluorescent reverse transcription polymerase chain reaction test for the qualitative detection of nucleic acid from the SARS-CoV-2 in upper respiratory specimens. Would potentially like insurance to cover the test. COVID Testing Summary Remember, if you have traveled to a designated Does medical insurance cover rapid covid test “hot spot” state in the last 14 days and need COVID testing, we may have to schedule a virtual appointment and allow our providers to advise you on next steps of care before presenting to the office. If you or anyone traveling with you is diagnosed with COVID abroad, then your travel insurance plan will provide cover against any medical expenses required for the treatment. Baggage Covers With airlines misplacing baggage so often, it's only right that there is a safeguard you can turn to. |
| CANT ACCESS EMAIL ON IPAD | 858 |
| How to disable pop-up blocker on mac chrome | How to play toto 4d |
| BREAKFAST IN SAN ANTONIO TEXAS DOWNTOWN | How to check booking status |

My swab did not go far up in my nose; is my test accurate?
What level do Yokais evolve at? - Yo-kai Aradrama Message